Medical Conditions Presenting as Psychiatric Symptoms
Author(s): Sheila Lahijani, MD, Kaleena Chilcote, MD
Editor(s): Donald Rosenstein, MD, Elizabeth Archer-Nanda, DNP
Introduction
Psychiatric symptoms and emergencies are common in patients with cancer due to the cancer itself, associated treatments, and other co-morbidities. Patients may develop a range of neuropsychiatric symptoms due to various causes, such as nutritional deficiencies, opportunistic infections, coagulopathies and/or bleeding, and central nervous system involvement. The management of cancer also frequently involves the necessary use of medications or other treatment modalities with neuropsychiatric side effects, such as corticosteroids. The risk of delirium is high in patients with cancer due to many possible causes, such as effects of cancer treatment, polypharmacy, sleep disruption, and prolonged hospitalizations. Patients needing time-sensitive medical and psychiatric evaluations should be triaged accordingly and followed up thereafter for further monitoring. Mental health clinicians taking care of patients undergoing cancer care should be knowledgeable about urgent symptoms, signs and syndromes that may develop and what type of management may be needed. Supportive care is often necessary, and this can include managing symptoms, eliminating underlying causes, and monitoring a patient’s response to interventions.
Table 1: Selected Etiologies of Neuropsychiatric Symptoms in Oncology
| Brain cancer |
Primary brain cancers (e.g., glioblastoma multiforme; CNS lymphoma) Metastatic brain cancer: Most prevalent in primary cancer of lung, breast, melanoma, colorectal, and renal cell Presenting symptoms vary depending on location: headaches (40-50%), focal neurological deficits (30-40%), cognitive impairment (30-35%), seizures (15-20%), stroke (5-10%) Diagnosed via brain MRI, ring-enhancing with surrounding edema |
| Leptomeningeal disease |
Dissemination of malignant cells through subarachnoid space Most prevalent in primary cancer of breast, lung, melanoma, GI malignancies, leukemia, lymphoma Most commonly involves base of the brain, Sylvian fissure, and cauda equina Presenting symptoms vary depending on location, related to increased intracranial pressure, meningeal irritation, and/or nerve disruption: headaches (30-50%), nausea/vomiting (25%), seizures (25%), leg weakness (21%), cerebellar dysfunction (17%), altered mental status (16%), cranial nerve involvement Diagnosed via brain MRI (sensitive), cerebrospinal fluid cytology (specific) |
| Paraneoplastic syndromes |
Immunologic factors directed toward antigens (either intracellular or cell surface/synaptic) that are expressed by tumor and healthy cells, leads to remote neurological effects Some clinical syndromes are well-documented (Lambert-Eaton Myasthenic Syndrome in 3% of small cell lung cancer Myasthenia gravis in 15% of thymomas, Limbic Encephalitis, Paraneoplastic Cerebellar Degeneration, Anti-NMDA Receptor Encephalitis) Diagnosed primarily by clinical syndrome, CSF and/or serum cytology (specific) 80% are diagnosed in people without a known cancer diagnosis |
| Tumor Lysis Syndrome |
Caused by cancer cell death leading to the release of intracellular contents Hyperuricemia and hyperphosphatemia lead to acute kidney injury High rates of delirium |
| Thiamine deficiency |
Wernicke encephalopathy describe the acute process and is a medical emergency Prevalence in oncology is unknown but suspected to be underdiagnosed: gastrointestinal cancers > hematologic cancers > gynecologic cancers > CNS cancers Classic triad of symptoms: encephalopathy, oculomotor abnormalities, and gait disturbance; most patients do not have all 3 Caine criteria for diagnosis in alcohol use disorder (not specifically studied in oncology): ≥2 of the following symptoms: dietary deficiency, oculomotor abnormalities, cerebellar dysfunction, AMS Rule of thumb: if there’s concern, treat it Use of 500 mg IV thiamine preferred over 100 mg PO during acute phase |
| Korsakoff syndrome describes chronic amnestic syndrome | |
| Hypothyroidism |
Can occur regardless of cancer status Potential side effect of immunotherapy agents and radiation; check thyroid function tests and collaborate with endocrinology for management |
| Adrenal insufficiency |
Can occur due to cancer or withdrawal of steroids Non-specificity of symptoms make it difficult to diagnose: weakness, nausea, vomiting, anorexia, dehydration Diagnosed by lab abnormalities in electrolytes (sodium, potassium, kidney function) |
Click here to view table as PDF
Table 2: Neuroleptic Malignant Syndrome (NMS) and Serotonin Toxicity (ST)
| Diagnosis | NMS | ST |
| Cause |
Dopamine antagonists Examples: antipsychotics, antiemetics |
Serotonergic agents: most cases are a result of two or more serotonergic agents used in combination Examples: antidepressants, buspirone, triptans, tramadol, St. John’s wort, cocaine, methylenedioxymethamphetamine (MDMA) , some antibiotics |
| Management | Stop offending agents | |
| Supportive care to manage hyperthermia, agitation, hydration, etc. | ||
| Benzodiazepines if sedation is necessary | ||
| Consider cyproheptadine | Consider dantrolene, bromocriptine | |
Click here to view table as PDF
Figure 1: Differentiating between NMS and SS
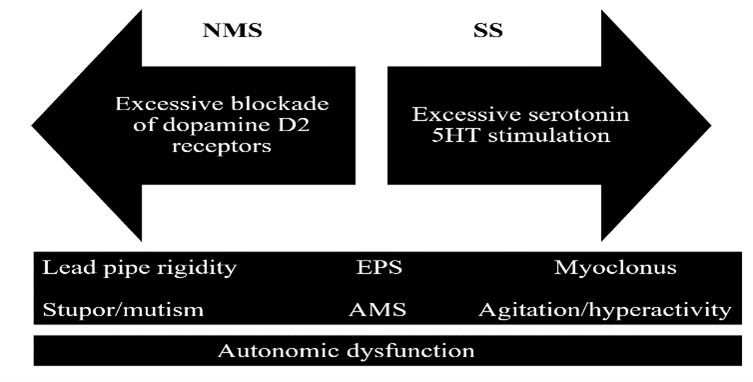
Table 3: Common Toxic Syndromes
| Toxidrome | Vital Signs | Pupils | Other | Example Causes |
| Cholinergic | ↓HR, ↑/↓BP | Miosis | AMS, lacrimation, salivation, urinary incontinence, vomiting, diarrhea, muscle fasciculations, seizures |
Organophosphates, pilocarpine, physostigmine, nicotine poisoning, Abrupt discontinuation of high dose anticholinergic agents |
| Anticholinergic | ↑HR, ↑BP, ↑T | Mydriasis | AMS, dry skin, urinary retention, decreased bowel wounds, myoclonus, seizures | Antihistamines, atropine, scopolamine, tricylic antidepressants |
| Hallucinogenic | ↑HR, ↑BP, ↑T | Mydriasis | AMS, hallucinations and illusions, depersonalization, nystagmus | LSD, mescaline, psilocybin |
| Sedative-hypnotic | N or ↓HR, ↓BP | Variable | AMS, hyporeflexia | Benzodiazepines, barbiturates, alcohol |
| Opioid | ↓HR, ↓BP, ↓RR | Miosis | AMS, hyporeflexia | Opioids |
HR, heart rate. BP, blood pressure. T, temperature.
Click here to view table as PDF
Table 4: Medications Commonly Used in Oncology and Neuropsychiatric Adverse Effects
| Medication | Side effects | Management Strategies |
| Corticosteroids | Anxiety, restlessness, insomnia |
Dose reduction if possible Benzodiazepines |
| Most common cause of hypomania/mania in cancer | Low dose atypical antipsychotics | |
| Antiemetics | Akathisia (psychomotor restlessness experienced internally in the legs) |
Minimize dopaminergic agents β-blockers, benzodiazepines |
| Cephalosporins | Delirium | Supportive care and symptom management; consideration of another antibiotic as per oncology team’s decision making |
| Opioids |
Toxicity-confusion, small pupils, slow breaths, cool skin, seizure Long-term use-bowel dysfunction, sleep disorders, hormonal disruptions, fractures |
Supportive care and symptom management Direct to emergency department if necessary Refer to pain specialist |
| Tamoxifen | Irritability, depression, insomnia |
Use of antidepressants; caution with strong CYP2D6 inhibitors serotonin norepinephrine reuptake inhibitors often used to target comorbid hot flashes and neuropathy; evidence based use of gabapentin is suggested |
| Interferon-alpha |
Depression Rare cases of mania |
Use of antidepressants Limited evidence for prophylactic use of antidepressants, presentation dependent |
| Chimeric antigen receptor t-cell therapy | Neurotoxicity related delirium (hypoactive or hyperactive) | Presentation dependent, often in hospital; no guidelines for treatment available at this time |
Click here to view table as PDF
Table 5: Catatonia
| Definition | Neuropsychiatric syndrome with motor, vocal, affective, and behavioral changes |
| Signs | Can include mutism, impoverished speech, stupor, increased motor tone, grimacing, muscle rigidity, autonomic instability |
| Causes | Cancer illness, medications (tacrolimus, cyclosporine, antibiotics), co-morbid mental illness, psychiatric medication or substance withdrawal |
| Diagnosis | Clinical exam and Bush-Francis Catatonia Rating Scale |
| Management | Supportive care, lorazepam, N-methyl-D-aspartate receptor antagonist, electroconvulsive therapy |
Click here to view table as PDF
Conclusion
Patients undergoing cancer care are at risk for developing neuropsychiatric symptoms and emergencies related to their medical conditions and their treatments. Frequently, patients are referred to mental health and behavioral health clinicians for depression, memory disturbances, and fatigue. While being familiar with the type of cancer and its treatment is important in understanding a patient’s presentation, having a structured approach to the diagnosis and management of different neuropsychiatric syndromes is critical to providing comprehensive care. Triaging urgent cases and collaborating with non-psychiatric colleagues highlights the multidisciplinary nature of psycho-oncology and promotes optimum cancer care. In settings without psychiatric providers, seeking out community providers, looking to members of national organization, and referring to the literature and resources are available can support further collaborative management of patients with cancer presenting with neuropsychiatric symptoms.

