Screening Measures
Introduction:
The goal of screening is to accurately identify patients who have distress and to rule out those who do not. Patients who have a positive screen are then referred for assistance when desired, with the aim of reducing distress. The term distress encompasses multiple domains (psychological, physical, social, spiritual) and clinicians may elect to screen for distress by targeting the construct(s) pertinent to their practice (for example, depression, spiritual distress, general distress, or all three). The choice of measures and procedures is based on the local context and available resources, in addition to national accreditation standards and guidelines. To ensure its appropriateness, a measure should be both valid (demonstrate it measures specifically what it purports to measure) and reliable (demonstrate it consistently measures the same construct from one time to another). To ensure its accuracy, a measure should demonstrate high rates of sensitivity (ability to detect true positives) and specificity (ability to rule out true negatives), with the caveat that there are tradeoffs between sensitivity and specificity. Researchers have developed and evaluated a number of screening measures to detect clinically significant distress. Table 2 presents measures that have been validated in diverse oncology populations and that comply with guidelines from various accrediting and certifying bodies such as the American College of Surgeons Commission on Cancer (CoC) and the NCCN. Cancer specific measures of fear of recurrence/progression and post-traumatic stress symptoms have not been widely adopted in distress screening, despite high prevalence of these problems in cancer populations, and thus are not included here. Additionally, items assessing patient’s interest and preferences in receiving care have not been routinely integrated to assist with triage/referrals.
Table 2. Candidate Screening Measures
| Screening Measure | Constructs assessed | Clinical Utility | # items | Unique Attributes | ||
| Severity score | Diagnostic case finding | Content validity* | ||||
|
Patient-Reported Outcomes Measurement Information System (PROMIS)8
|
Depression, anxiety, physical function, fatigue, pain, pain interference, ability to participate in social roles and activities, and sleep disturbance.
Many more constructs available. |
x | x | x |
4-8 items per construct
Reduced item, ultra-short versions available
|
Rigorous validity and reliability
High sensitivity and specificity
EPIC integration available
CAT** available to reduce patient response burden (lower content validity) |
|
Edmonton Symptom Assessment System (ESAS)9
|
Depression, anxiety, pain, tiredness, drowsiness, nausea, lack of appetite, shortness of breath, overall well-being (and a fill in the blank item) | x | x | 10 total, 1 item per construct |
Single item per construct — relies on individual patient definition of construct
Includes nausea and appetite
Includes fill in the blank item for patient identified symptom
Includes bodily location
|
|
|
Patient Health Questionnaire (PHQ-9), General Anxiety Disorder scale (GAD-7)10
|
Depression, Anxiety
|
x | x | x |
9, 7
Reduced item, ultra-short versions available
|
Suicide item included in PHQ-9
|
|
Hospital Anxiety and Depression Scale (HADS)11
|
Depression, Anxiety | x | x | x | 14 (7 items for each) | |
|
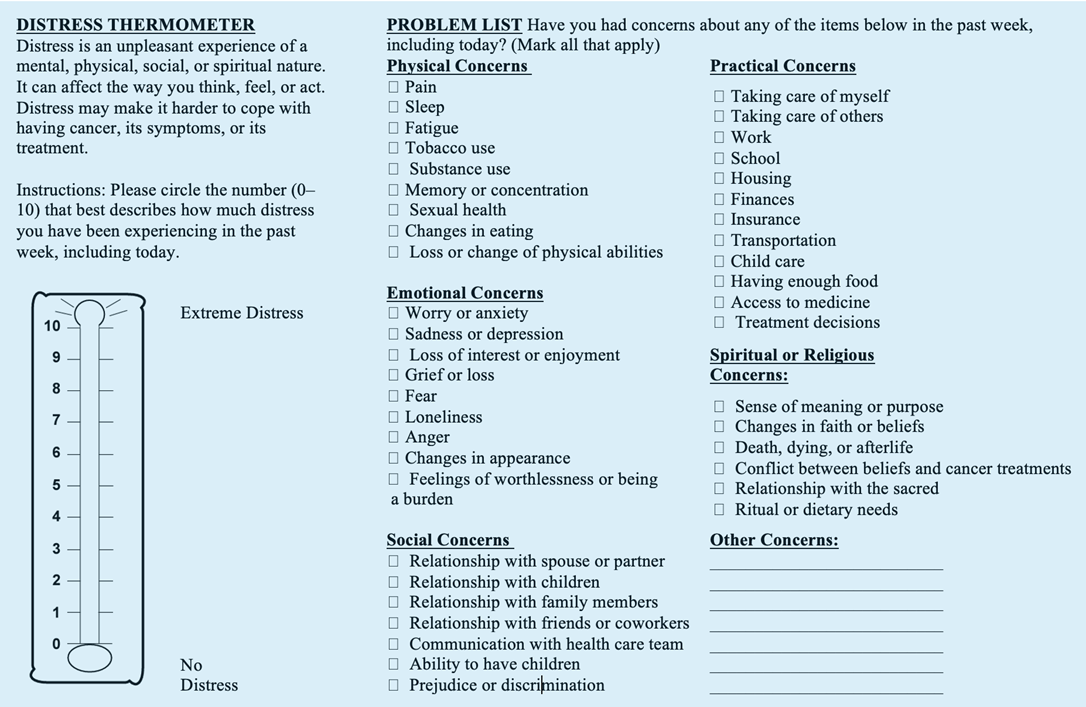
NCCN Distress Thermometer (DT)3,12
|
General distress + problem checklist | x | 1 + multi-item problem checklist |
Low specificity, positive screens require further assessment due to low case-finding utility.
|
||
|
Religious and Spiritual Struggles Scale (RSS)13
|
Religious and spiritual distress | x | 26 |
Comprehensive assessment of 6 sub-domains of religious and spiritual distress
|
||
*Content validity requires several items to fully assess the “symptom content” of a single construct. As the number of items for each construct decreases, core symptoms are left out and content validity and specificity naturally decrease. As a consequence of low content validity, the need for downstream clinician time and effort increases in the form of assessment and interview. Thus, ultra-short measures (<=5 items) tend to have lower content validity and specificity than short measures (<15 items).14
**CAT- Computerized Adaptive Testing
Click here to view table as PDF
Figure 1. Edmonton Symptom Assessment System

Figure 2. NCCN Distress Thermometer and Problem List