Models of Care in Psychosocial Oncology
Author(s): Julia Ruark, MD MPH, Jesse Fann, MD MPH, Michael Sharpe, MA MD
Editor(s): Jesse Fann, MD, Joseph Greer, PhD
INTRODUCTION
For oncology services to treat the whole patient and not just their cancer, they must offer biopsychosocial care that meets the needs of the whole person.
This chapter offers evidence-based and practical guidance on how to provide that care by integrating a psychosocial oncology component into a cancer care program.
PRINCIPLES AND APPROACHES
To address psychosocial needs requires both identification and intervention. Identification by screening for distress is a useful start. However, a system to ensure the appropriate triage, treatment, and follow-up of individuals is required in order to improve patient outcomes.(1)
The principles of integrated care are shown in Table 1.(1,2)
Table 1. Principles of Psychosocial Model of Care integrated into Cancer Care
| Principle 1 |
Population-based -use of universal distress screening -use of patient registries to track patient population and outcomes |
| Principle 2 |
Level of clinical expertise matched to patient needs -mild distress treated with low intensity & less costly interventions -significant distress (e.g., major depression, severe anxiety) given more intensive treatment |
| Principle 3 |
Patient-centered -use of patient-centered outcomes (e.g., patient-reported outcomes) to guide a stepped care approach -use shared-decision making and culturally sensitive approaches |
| Principle 4 |
Evidence-based treatment delivered in timely fashion & across the continuum of cancer care -positive screenings trigger immediate assessment and treatment -screening occurs at multiple time points during cancer journey -measurement-based care at initial and follow up visits (e.g., PHQ9, GAD7) guide treatment to target |
Click here to view table as PDF
The degree of integration of the psychosocial components of care into cancer care is not ‘all or nothing’ but can be described as being on a continuum from completely separate services to full integration (Table 2).
Table 2. SAMHSA-HRSA Levels of Integration of Health Care Systems (Adapted from ref 3)
|
Level 1 Minimal Collaboration |
Level 2 Basic Collaboration at a Distance |
Level 3 Basic Collaboration Onsite |
Level 4 Close Collaboration Onsite with Some Integration |
Level 5 Close Collaboration Approaching Integration |
Level 6 Full Collaboration with Full Integration |
Click here to view table as PDF
Approaches to delivering a psychosocial component of care
A variety of approaches have been taken to integrating psychosocial care into cancer care. Each have advantages and disadvantages, which are shown in Tables 3a & 3b.
Table 3a. Models of psychosocial care – oncology outpatients.
Provider=Mental health provider.
| Model of Care | Description | Advantages |
Disadvantages
|
| Off-site referral | Provider outside of cancer center; receives referral from oncology team or patient self-refers | No cost to cancer center |
Minority of patients follow through with outside referrals. Few providers with oncology expertise. High risk of inadequate treatment
|
| Co-located provider | Provider located within the clinic; often available for limited number of visits |
Warm-hand offs Increased access |
Limited availability of follow-ups. Risk of inadequate treatment. Often limited collaboration with oncology team due to capacity constraints
|
| Joint clinics | Provider & oncologist see patient together | Highly integrated Acceptable to patients |
Costly. Only cost effective for patients with complex problems
|
|
Collaborative Care
|
Systematic screening followed by engagement with care manager who is a member of oncology team |
Cost-effective Highly integrated Population based Strong evidence for improving outcomes |
Initial cost of setup. Requires system changes to create & sustain
|
| Fully Integrated Oncology Team | Psychosocial providers work as members of outpatient oncology team |
Highly integrated Highly acceptable to patients |
Costly. Not feasible in most settings |
Click here to view table as PDF
Table 3b. Models of psychosocial care – oncology inpatients
| Model of Care | Description | Advantage |
Disadvantage
|
| Consult Service |
Oncology team refers to outside psychosocial consultation service
|
No cost to cancer center |
Often inefficient and fragmented. May not be effective due to lack of oncology expertise
|
|
Co-located psychosocial provider
|
Referrals to a psychosocial team co-located within oncology inpatient unit |
Relatively acceptable to patients. Can educate oncology team. |
Will not meet population needs. May lack oncology expertise.
|
|
Proactive Inpatient Consultation |
Systematic screening of all patients and active treatment of needs by dedicated team | Captures whole inpatient population. Likely cost-effective . |
Requires system changes to create & sustain. Not fully integrated
|
| Fully integrated psychosocial care |
Psychosocial providers work as members of the oncology inpatient team
|
Highly integrated. Can upskill staff. Highly acceptable to patients
|
Costly. Not feasible in most settings. |
Click here to view table as PDF
Which of these models, or combination of models, is best for a specific cancer program depends on the ambition of the program (e.g., how integrated and comprehensive you want the service to be), the resources that can be identified (e.g., funding, space, staffing and technologies available), and scope (e.g., whether you want to cover both inpatient and outpatient clinics and at how many sites).
Recommended model for outpatient oncology care
For outpatient oncology care, the Collaborative Care Model has the strongest evidence for cost-effectively improving patient outcomes.
- There is particularly strong evidence for its role in improving outcomes for patients with comorbid major depression in the cancer care setting (4) and it has been adapted for patients with a wide range of behavioral health conditions, including those with anxiety, PTSD, substance use disorders, and serious mental illness. The model is also adaptable for use with telehealth technologies.
- Collaborative care is a population-based model that identifies patient needs by systematic screening.
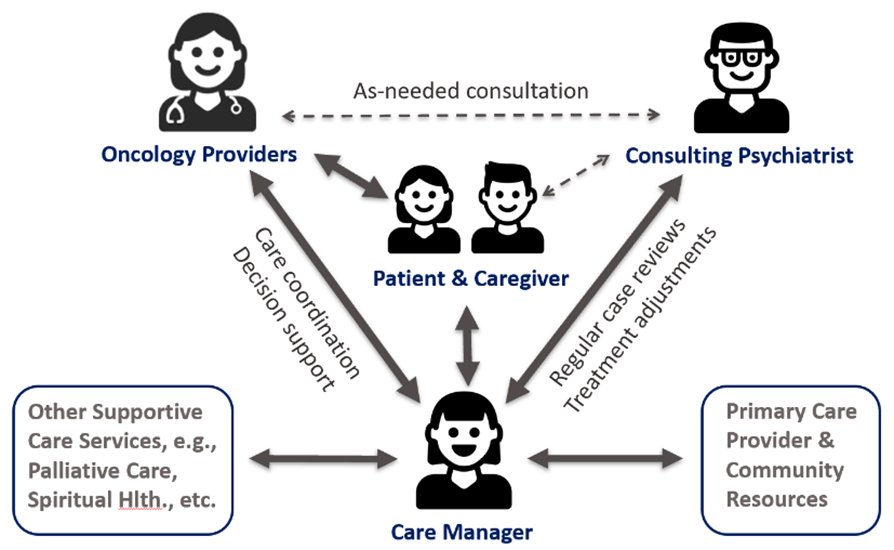
- The cornerstone of intervention in collaborative care is the integration of a care manager (often a clinical social worker or nurse) located within the oncology clinic and a consulting psychiatrist, who can be co-located or remotely located. See Figure 1.
- The care manager receives specialized training and works closely both with patients and with other members of the multidisciplinary oncology team. The care manager tracks their caseload on a registry and provides the majority of psychosocial interventions to the patient, including a therapeutic relationship, care coordination, referral to other support services and community resources, and brief, evidence-based psychotherapy (e.g., behavioral activation, problem-solving treatment).(5)
- The consulting psychiatrist reviews the care manager’s cases regularly (typically weekly) to monitor progress and develop and adjust treatment plans with the care manager. If medication management is advised, the psychiatrist can provide recommendations indirectly, which the oncologist prescribes. If specialty mental health care is clinically indicated and availability allows, the patient can be referred for direct consultation to the psychiatrist or a psychologist.
- There are billing codes by the Centers for Medicare and Medicaid Services (CMS) that support reimbursement for collaborative care.
Figure 1: Collaborative care model structure
Recommended model for inpatient oncology care
For inpatient oncology care the Proactive Consultation Model (6) This is the equivalent of collaborative care for the needs of hospital inpatients. It is based on proactive systematic screening for psychosocial needs, rather than oncologist referral, with active interventions by psychosocial clinicians to address those needs with outcome monitoring and discharge planning. There is growing evidence for its cost-effectiveness in a variety of specialist inpatient settings, but more research is required including in oncology
- Like collaborative care, the proactive consultation model seeks to address the needs of the whole (inpatient) population by using systematic screening of patients. The nature of the screening will depend on whether the service seeks to focus on psychiatric illness or wider needs. Screening can be based on review of records and mental health screening measures, or on individual patient assessment.
- As the complexity of inpatients is generally high, there is a greater role for the C-L psychiatrist in directing patient care than in outpatient collaborative care. However, as with collaborative care, the number of patients the psychiatrist can manage is extended by the use of nurses or physician assistants who provide much of the direct patient care, under the psychiatrist’s supervision.
- Planning for hospital discharge and linking with outpatient services to continue care for problems identified in hospital aims to reduce inpatient length of stay.
Cultural Considerations
BIPOC and LGBTQ communities with cancer have high rates of mental illness and yet have less access to care. Integrated psychosocial care is a potential solution for improving access and outcomes in these populations. There is some evidence supporting its efficacy in doing this, but more is needed (7). Members of BIPOC & LGBTQ communities may have experienced poor treatment by previous psychosocial providers. Thus, it is important that active efforts are made, within your chosen model of care, to engage patients from these communities in a culturally sensitive manner.
The implementation of new services
To implement a psychosocial component to oncology care, the following factors have been found to be important (8):
- Determine what is the appropriate model of care for your oncology practice
- Communicate a clear vision of what the model can achieve for patients and clinicians
- Identify champions (including from oncology, social work, psychiatry) to advocate the model to administrative leadership and clinicians
- Create a practical and detailed business plan and timeline for implementation, often starting with a pilot phase
- Engage an expert to advise on the implementation process
- Access resources such as the American Medical Association behavioral health integration resources (https://www.ama-assn.org/delivering-care/public-health/compendium-behavioral-health-integration-resources-physician) or the University of Washington AIMS Center (https://aims.uw.edu/)
CONCLUSION
Psychosocial care is an essential component of cancer care. There are a number of available service models to consider. The most effective models provide timely, integrated and evidenced-based care in a population-based approach along the whole continuum of cancer care.
For outpatient oncology services, collaborative care is the most evidenced-based model of care. For inpatient oncology care, a similar model called proactive psychiatric consultation shows promise. Implementation of these systematic and integrated service models takes time and resources. We recommend careful advance planning and the engagement of an expert for successful implementation.
REFERENCES
1. Pirl W, Greer J, & Wells-Di Gregorio S, et al. Framework for planning the delivery of psychosocial oncology services: an American psychosocial oncology society task report. Psycho-Oncology. 2020; 29:982-1987.
2. Fann J, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012; 30(11):1178–1186.
3. Heath, B. Wise Romero, P, K. Reynolds. A standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions. 2013.
4. Li M, Kennedy EB, Byrne N, et al. Systematic review and meta-analysis of collaborative care interventions for depression in patients with cancer. Psycho-Oncology. 2017; 26(5):573-587.
5. Courtnage T, Bates NE, Armstrong AA, et al. Enhancing integrated psychosocial oncology through leveraging the oncology social worker’s role in collaborative care. Psycho-Oncology. 2020; 29:2084-2090.
6. Oldham MA, Chahal K, Lee HB. A systematic review of proactive psychiatric consultation on hospital length of stay. Gen Hosp Psychiatry. 2019; 60:120-126.
7. Ell K, Xie B, Kapetanovic S, et al. One-year follow-up of collaborative depression care for low-income, predominantly Hispanic patients with cancer. Psychiatr Serv. 2011; 62(2):162–170.
8. Walker J, Hobbs H, Wanat M, et al. Implementing collaborative care for major depression in a cancer center: an observation study using mixed-methods. Gen Hosp Psychiatry. 2022; 76: 3-15.

